First-ever lab-grown blood could change medicine forever
For the first time ever, scientists have given patients red blood cells that were grown in a lab. This feat is part of a clinical trial in England looking into the safety of the cutting-edge technique, which could help tackle the ongoing blood supply shortage that was worsened by the pandemic.
The trial is a collaboration between institutions including the University of Bristol, the University of Cambridge, and the National Health Service.
Regular transfusions can be life-saving for people with conditions like sickle cell disease, which affects the shape of red blood cells and can block blood flow, and thalassemia, which causes the body to produce too little of a protein called hemoglobin.
Now, these lab-grown red blood cells could stretch sparse donations into larger volumes. The procedure could also help address the need for more blood from Black donors — sickle cell disease is prevalent among Black people, and blood is most compatible when donated from people of the same race or similar ethnicity.
And unlike donor blood, which can contain relatively old cells, these lab-grown cells are guaranteed to be fresh. This means they can last longer and perform better, reducing the need for frequent transfusions. When people receive lots of transfusions, they also run the risk of developing too much iron in their bodies.
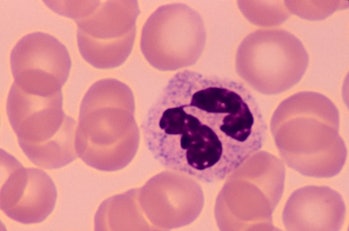
A white blood cell surrounded by red blood cells, which scientists have figured out how to grow in the lab.Ed Reschke/Photodisc/Getty Images
How to grow blood cells — The scientists started with a regular blood donation and used magnetic beads to pinpoint the flexible stem cells that can morph into red blood cells, CNBC reported.
Then, they put the stem cells in a nutrient solution for 18 to 21 days, which nudges the cells to proliferate and grow into more mature cells, according to The Guardian. Then, they tagged the cells with a radioactive substance to track them in blood samples from trial participants over the six months following the first injection of cells.
So far, two healthy volunteers have received the lab-grown red blood cells, and they haven’t reported any negative side effects. Next up, the team will give a minimum of 10 participants two “mini” transfusions at least four months apart — one consisting of standard donated red blood cells and another composed of lab-grown ones.
The researchers will analyze patient blood samples to determine whether the lab-grown red blood cells will last longer than the ones made in the body. While further research is needed, this marks a major step forward in treating blood disorders.
“The need for normal blood donations to provide the vast majority of blood will remain,” says Farrukh Shah, the medical director of tranfusion at NHS Blood and Transplant. “But the potential for this work to benefit hard-to-transfuse patients is very significant.”
Read more about the trial here.
CONTINUE HERE: https://www.inverse.com/innovation/lab-grown-red-blood-cells?utm_campaign=44338&utm_medium=inverse&utm_source=newsletter&utm_session=d5783603-487e-4b5e-a91c-97dbf2fe0147
For the first time ever, scientists have given patients red blood cells that were grown in a lab. This feat is part of a clinical trial in England looking into the safety of the cutting-edge technique, which could help tackle the ongoing blood supply shortage that was worsened by the pandemic.
The trial is a collaboration between institutions including the University of Bristol, the University of Cambridge, and the National Health Service.
Regular transfusions can be life-saving for people with conditions like sickle cell disease, which affects the shape of red blood cells and can block blood flow, and thalassemia, which causes the body to produce too little of a protein called hemoglobin.
Now, these lab-grown red blood cells could stretch sparse donations into larger volumes. The procedure could also help address the need for more blood from Black donors — sickle cell disease is prevalent among Black people, and blood is most compatible when donated from people of the same race or similar ethnicity.
And unlike donor blood, which can contain relatively old cells, these lab-grown cells are guaranteed to be fresh. This means they can last longer and perform better, reducing the need for frequent transfusions. When people receive lots of transfusions, they also run the risk of developing too much iron in their bodies.
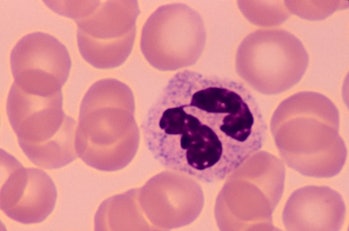
A white blood cell surrounded by red blood cells, which scientists have figured out how to grow in the lab.Ed Reschke/Photodisc/Getty Images
How to grow blood cells — The scientists started with a regular blood donation and used magnetic beads to pinpoint the flexible stem cells that can morph into red blood cells, CNBC reported.
Then, they put the stem cells in a nutrient solution for 18 to 21 days, which nudges the cells to proliferate and grow into more mature cells, according to The Guardian. Then, they tagged the cells with a radioactive substance to track them in blood samples from trial participants over the six months following the first injection of cells.
So far, two healthy volunteers have received the lab-grown red blood cells, and they haven’t reported any negative side effects. Next up, the team will give a minimum of 10 participants two “mini” transfusions at least four months apart — one consisting of standard donated red blood cells and another composed of lab-grown ones.
The researchers will analyze patient blood samples to determine whether the lab-grown red blood cells will last longer than the ones made in the body. While further research is needed, this marks a major step forward in treating blood disorders.
“The need for normal blood donations to provide the vast majority of blood will remain,” says Farrukh Shah, the medical director of tranfusion at NHS Blood and Transplant. “But the potential for this work to benefit hard-to-transfuse patients is very significant.”
Read more about the trial here.
CONTINUE HERE: https://www.inverse.com/innovation/lab-grown-red-blood-cells?utm_campaign=44338&utm_medium=inverse&utm_source=newsletter&utm_session=d5783603-487e-4b5e-a91c-97dbf2fe0147





 Sat Mar 23, 2024 11:33 pm by globalturbo
Sat Mar 23, 2024 11:33 pm by globalturbo

